Relationship between periodontal diseases and preterm birth: Recent epidemiological and biological data
Abstract
Preterm infants are born prior to completion of 37 weeks of gestation. These patients are seen on the rise despite the efforts put in to control them. Global incidence of preterm birth is around 9.6% of all birth representing 12.9 million births with regional disparities: From 12% to 13% in USA, from 5% to 9% in Europe, and 18% in Africa. First reported by Offenbacher et al. in 1996 relationship exist between maternal periodontal disease and delivery of a preterm infant. This article reviews the recent epidemiological and biological data. The articles were searched on Google, PubMed recent articles were selected. Mainly, three hypotheses by which periodontal bacteria can affect the outcome of pregnancy. Biological hypothesis: (a) Bacterial spreading, (b) Inflammatory products dissemination, (c) Role of fetomaternal immune response against oral pathogens. The promotion of the early detection and treatments of periodontal disease in young women before and during pregnancy will be beneficial especially for women at risk.
Introduction
Preterm infants are born prior to completion of 37 weeks of gestation.[1,2] An estimated 11% of pregnancies end in preterm birth (PB),[3] and this rate appears to be on the rise in several developed countries, despite significant advances in obstetric medicine and improvements in prenatal care utilization. Of particular interest are the very preterm infants, born prior to 32 gestational weeks, the majority of which require neonatal intensive care due to their increased perinatal mortality, primarily due to impaired lung development and function. Still, the overall contribution of PB to infant mortality and morbidity is substantial and includes a number of acute and chronic disorders including respiratory distress syndrome, cerebral palsy, pathologic heart conditions, epilepsy, blindness, and severe learning disabilities.
This article looks into recent view of the relationship between PB, preterm birth associated to low-birth weight (PBLW) and periodontal disease. The selection of article was done by Google and PubMed search for the topic and both pro and against articles was considered.
Periodontal Health and Pregnancy: A Reciprocal Relationship
Global incidence of PB is around 9.6% of all birth representing 12.9 million births,[4] with regional disparities: From 12% to 13% in USA, from 5% to 9% in Europe, and 18% in Africa. For 10 years, the rate of PB does not decrease in most of the industrialized countries. In USA, PB prevalence increased from 9.5% in 1981 to 12.7% in 2005. Furthermore, women classified as black, Afro-American and Afro-Caribbean, are frequently reported to be at higher risk of PB.[5] PB rates are in the range of 16–18% in black women compared with 5–9% for white women in USA.[6]
In India, the incidence of PB has been reported to be 14.5%.[7] PB is a public health problem because it is associated with high perinatal morbidity and mortality, long-term neurodevelopmental disabilities and poor respiratory outcome.[8] Gopichandran et al.[9] in 2010 reported the psychological factors during pregnancies in a study conducted in rural South India maternal stress due to pregnancy-related anxiety, stressful life events, death of a spouse, depression during pregnancy and poor self-esteem are risk factors for preterm labor.[10] Levels of stress for a pregnant woman are likely to be much higher in resource-poor settings such as India. Many preventive treatments have been proposed to decrease the risk of PB especially for women at risk. Many countries have programs offering special assistance to these women including advice and counseling (about nutrition, drugs, tobacco), assistance (transportation to clinic appointments, household help), and emotional support.[11] Obstetric treatments are possible including treatment with tocolytic agents, antenatal corticosteroids and antibiotics, and optimum timing of indicated PB. These measures are intended to reduce the burden of prematurity-related illness more than to reduce the rate of PB and have effects on perinatal morbidity.[12] Hunter, in 1910 thru his “Focal infection theory” was first to point out the possibility that the pathogenic microorganisms and their products from infectious foci can spread to other parts of the body and trigger different diseases. Thoroughly criticized by his contemporary’s for lack of adequate evidence to support his credentials, it was dumped and discarded. Improvements in epidemiology, biostatistics, and molecular biology in the last three decades and the concern among dental researchers to assess the effects of the mouth on general health led to the rehabilitation of the Hunters theory.[13]
Offenbacher et al.,[14] in 1996 first reported a relationship between maternal periodontal disease and delivery of a preterm infant. Periodontal disease is a Gram-negative anaerobic infection of the mouth that affects up to 90% of the population and has been demonstrated to be higher in pregnant women. The 1996 study by Offenbacher[15] and colleagues suggested that maternal periodontal disease was associated with a seven-fold increased risk of delivery of a PLBW infant. These authors concluded that about 18% of PLBW cases might be attributable to periodontal disease. After controlling for known risk factors, the results of this study was the first to show that periodontitis was a significant risk factor for PLBW. Rajakapse et al.[16] confirmed this finding by showing that women with healthy periodontal status had a lower risk of having adverse pregnancy out-comes.
Preeclampsia is characterized by a systemic vascular dysfunction that affects placental circulation, as demonstrated by histopathology changes. Indeed of been considered a multifactorial illness, there is growing evidence of the presence of chronic infection as etiological/or triggering factor for systemic vascular dysfunction (endothelial dysfunction). Previous studies observed an association between periodontal illnesses and preeclampsia.[4,5,6,7]
The current article aims to provide insight into studies regarding periodontal disease as a possible risk factor for adverse pregnancy outcomes.
Epidemiological Link
During the last decade, numerous epidemiological studies have been conducted on the association between PB and periodontitis.[17] More or less strong associations between periodontal status and PB alone, low birth weight (LBW), or PLBW have been shown in cohort/cross-sectional studies by Lunardelli and Peres,[18] (Brazil, PB P < 0.02), Offenbacher et al.[19] (USA, PB P = 0.013), Lopez et al.[20] (Chile, PLBW P < 0.0004 and RR = 3.5), Siqueira et al.[21] (Brazil, PB P < 0.001), Rajapakse[16] (Sri Lanka, PB odds ratio [OR] =2.3), Toygar et al.[22] (Turkey, PB and PLBW P < 0.01), Agueda et al.[23] (Spain, PB OR = 1.77), and Heimonen et al.[24] (Finland, PB P < 0.001), and also in case-control studies by Gomes-Filho et al.[25] (Brazil, PLBW OR = 2.1), and Khader et al.[26] (Jordan, PLBW P < 0.0001).
However, some other investigations did not find a significant association, such as cohort studies by Moore et al.,[27] Noack et al.,[28] Agueda et al.,[23] Nabet et al.,[29] and case-control studies by Davenport et al.,[30] Bassani et al.,[31] andVettore et al.[32]
The different conclusions of these studies could be explained by the use of different definitions of adverse pregnancy outcomes, for instance, pre term birth versus preterm low-birth weight and periodontal disease definitions, reflecting, in fact, different pathologic entities and disease severities.[33,34] Indeed, the periodontal status assessment of pregnant women is mainly based on threshold numbers of sites with pre specified values of periodontal pocket depth and/or clinical attachment loss,[18,19,20,23,25,35] but could also be determined by the use of other composite index such as Community Periodontal Index for Treatment Need.[24,30] or other clinical signs, including bleeding on probing.[16] Interestingly, the use of variable periodontitis definitions could reverse the association in some cases, especially in cohort studies.[32,34] However, a high prevalence of severe periodontitis is frequently associated with PB and/or PLBW,[21,23,25,35] while a low prevalence (7.2%) is not.[27]
Furthermore, the strength of the association between periodontal disease and PB incidence increases frequently with the severity of periodontitis,[19,25,31,34] All these data suggest that women populations with a high prevalence of severe periodontitis are at risk for PB.
Biological Hypothesis
Considering epidemiological evidence, biological theories have been proposed to link PB and periodontal diseases.[20] Mainly, three hypotheses are developed – Bacterial spreading; Inflammatory products dissemination; and Role of fetomaternal immune response against oral pathogens.
Bacterial spreading
The current paradigm indicates that the majority of intrauterine infection originates in the lower genital tract.[36] Despite this statement, number of studies report intrauterine infections caused by those species, which are not found in the urogenital tract. The bacterial spreading theory is based on the possible dissemination of oral bacteria including periodontal pathogens through blood circulation to the amniotic fluid and leading to chorioamniotic infections.[37] The frequent gingival inflammation of women presenting periodontal diseases especially the pregnancy associated gingivitis,[38] facilitates bacteremia process. Furthermore, the more periodontal pockets are deep, the more important is the exchange surface between bacteria biofilm and blood circulation (15–20 cm2 in the most severe cases).[39] Many analyses of amniotic fluid or placenta have been performed and evidence the presence of different oral pathogens such as Bergeyella, Eikenella,[36] Fusobacterium nucleatum, or Porphyromonas gingivalis.[40,41,42]
Inside uterus, these pathogens could provoke an inflammatory response. The increase of inflammatory cytokines or metalloproteases synthesis and the neutrophil activation could induce PB process.[36]
In vivo studies show that the invasiveness of uterine tissues largely depends on the type of bacteria. Potential pathological mechanisms of certain periopathogens, especially for P. gingivalis and F. nucleatum, have been studied. For example, P. gingivalis could infect syncytiotrophoblasts, chorionic trophoblasts, decidual cells, and amniotic epithelial cells,[42] and promotes inflammatory process trough Toll-like receptor 4.[43]
Finally, a case-report study has been published in 2010 concerning a stillbirth caused by F. nucleatum from the mother’s mouth.[44] This study highlights the fact that an oral periodontal pathogen can, by hematologic pathway, colonize placenta and provoke fetal complications. It is important to notice that such colonization may be dependent from mother’s immunological status.
Hematogenous dissemination of inflammatory products
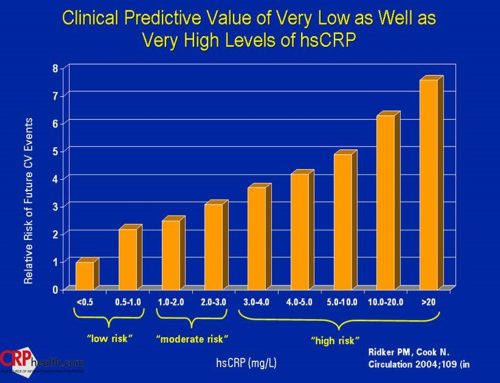
Acute inflammation is responsible for a substantial fraction of PB.[45] In 1998, Offenbacher et al.[46] suggested that the cytokines produced by local inflammation in periodontal tissues affected by periodontitis have systemic effects after diffusion of such cytokines through blood flow. Locally, studies show that periodontal diseases increase secretion of several cytokines, notably prostaglandin E2 (PGE-2), tumor necrosis factor-α, interleukin 6 (IL-6) or interleukin 1β (IL-1β).[47,48] Analysis of amniotic fluid obtained at the time of PB shows elevated levels of inflammatory cytokines.[49] It can be hypothesize that cytokines produced in periodontal tissues promote inflammation in maternal-fetal unit. Clinically, high-gingival crevicular fluid levels of PGE-2, IL-1β, or IL-6 have been associated with their elevated levels in amniotic fluid.[46] The inflammatory response appears to be the privileged pathway of the pathogenic periodontal disease influence on pregnancy, as suggested for other major systemic diseases, including cardiovascular diseases or diabetes.[50]
Role of fetomaternal immune response
The immune and genetic characteristics of the fetus and pregnant women are one of the potential mechanisms linking periodontal diseases to PB. Numerous studies have analyzed fetal and maternal antibodies directed against oral pathogens during pregnancy. In the study of Boggess et al.,[51] 35.2% of samples are IgM positive for at least one oral pathogen, and 26.6% are positive for more than one. The presence of IgM is associated to an increased risk of PB. This immune response against oral pathogens could be associated with an inflammatory response, and the synergy between the two mechanisms increases significantly the risk. The mechanisms linking periodontal diseases and PB are not well defined. Further investigations should be performed to evaluate the impact of each theory. Nevertheless, it can be hypothesized that the influence of periodontal diseases on PB is the result of inflammation of the fetomaternal unit that is amplified in women presenting particular phenotype.
Effects of Periodontal Treatment on Preterm Birth Incidence
Considering periodontal diseases as a risk factor for PB, interventional studies have been performed to evaluate the impact of periodontal treatment on pregnancy outcomes. Case-control studies including a relative large number of pregnant women (>400) show some apparent contradictory results and different conclusions.[20,52,53,54,55,56] Indeed, the periodontal treatment may improve periodontal conditions and or pregnancy outcomes or not.[53,55] A recent meta-analysis indicates that the treatment of periodontal diseases does not reduce the rate of PB.[57] However, as discussed above for epidemiological studies, the conclusions of this analysis could be balanced by the relative heterogeneity of studied populations, according to risk factors ethnicity, smoking, socio-educative levels, and periodontal status definition. For instance, the percentage of black people varies considerably between studies: 50–65% of Hispanic and Caucasian;[20,58] 45–87% of Afro-American.[52,55] Furthermore, the modalities of periodontal care in the different studies display some differences that may influence periodontal outcomes. A first session of etiologic periodontal treatment, including oral hygiene instructions, scaling, and root planning was generally performed at the end of the first trimester of pregnancy (before 20–28 weeks). This first session could be unique,[53,55] or reinforced by regular control visits and complementary treatments if necessary until delivery.[20,52] The local effects of periodontal treatments are generally positive. Gingival inflammation and mean probing pocket depth are reduced, especially in the study using reinforced periodontal treatment modalities. However, a relative high rate of patients demonstrating a periodontitis progression is observed in some studies 70%,[49], 50%,[48] and 68%,[56] suggesting that periodontal treatments do not work so efficiently than in a general population.[53] Indeed, the relative “narrow therapeutic window” to perform periodontal treatment and to obtain a successful periodontal lesion cicatrization, and the aggressive profile of severe periodontitis in young women could be considered as limiting factors.[53,56] A recent study performed by Jeffcoat et al.,[56] confirms that the efficiency of periodontal treatment should be considered before the analysis of results. In this study, 322 pregnant women with periodontal disease have been followed, 160 have received randomly complete periodontal treatment, and 162 have served as control without treatment. No significant difference was found in the term of PB incidence between the two groups. However, after considering the effect of periodontal therapy, the results demonstrate a strong and significant relationship between successful periodontal treatment and full-term birth ratio (OR = 6.02).
Despite apparent conflicting data, the majority of studies report that periodontal treatment is safe for pregnant women and improve periodontal status.[52,54,56] A pregnant woman is a particular patient. In order to decrease the impact of periodontal disease on PB incidence, the early diagnosis promotion of periodontal disease for young women especially for those presenting major risk factors should be recommended.
Conclusion
Periodontal diseases appear to be a potential risk factor for PB. As well as other modifiable risk factors, these diseases must be taken in charge. Cooperation between obstetricians or general practitioners and periodontists should be developed. The promotion of the early detection and treatments of periodontal disease in young women before and during pregnancy will be beneficial, especially for women at risk.



Leave A Comment
You must be logged in to post a comment.